Information Day 2019
From 10:00 – Registration, with Coffee on Arrival
Everyone was asked to write what they hoped to get out of the day on a post-it note (Hopes for the Day) which were gathered together into rough groups to form the topics for the break-out sessions.
10:30 – Welcome, Domestics and Introductions – Laura Dunn: Kangaroo Club Chairman
Laura began by welcoming all the attendees and introducing the committee members. The day was dedicated to Martin Brandt who sadly had passed away since the last Information Day. Martin was Secretary of the Kangaroo Club for many years and worked tirelessly for the club.
11:00 – Pouch Surveillance and The Future of Pouch Surgery – Mr Jonathan Gosling: Colorectal Registrar, OUH NHS Foundation Trust
Jonathan Gosling started by introducing himself and explaining that for the last year he had been working at OUH NHS Foundation Trust as a registrar with Mr Bruce George, but he had just (three days before the Information Day) started at St Marks Hospital, London.
He then gave two presentations.
1. Pouch Surveillance
Mr Gosling started by explaining that pouch surveillance is for people with pouches who are well, it involves having a camera exam of the pouch and a Gastroscope of the pouch, cuff and the first section of the small bowel. This can be done in one day and commonly no sedation is required, although you can have sedation if you would like it. Photos and samples of tissues are taken from the anus, the small section of the rectal cuff and the small bowel that comes into the pouch.
Mr Gosling went on to explain that pouches require surveillance for two main reasons.
• To explore the potential for optimizing pouch function
People with pouches can experience a narrowing and inflammation in the small bowel loop before the pouch, the pouch rectal cuff and the anal canal, and if it is looked at it can be better treated, and this treatment can be optimized.
• The retained section of rectum can undergo changes and (rarely) become cancerous
Although it is important to continue to monitor the pouch and rectum for changes this is very unlikely. In fact, a Dutch study looked at 2,000 pouches over 12 years and found they had a 1/1000 chance of becoming cancerous which is less than the general populations’ risk of colorectal cancer.
We then learnt about the international guidelines for pouch surveillance, which are quite variable. The AGA (American) guidelines do not have any specific guidelines on pouch surveillance, the BSG (British) guidelines recommend yearly examinations in high-risk patients or every five years in low-risk patients and the ASGG and ECCO (European and other American guidelines) recommend yearly examinations in high-risk patients or not at all. A patient is considered high risk if when their colon is removed it has cancerous changes, polyposis syndromes, if they have liver problems associated with Ulcerative Colitis, or their pouch is constantly inflamed.
In practice this varies widely, a recent survey showed that 8/10 pouches required surveillance, but the frequency varied hugely. Out of 300 pouches 30% had never had any surveillance and the other 70% hadn’t had a proctoscopy. In Oxford patients are advised to have a proctoscopy every three years, which increases to once a year if they have high risk features.
Mr Gosling told us that the aim of this talk was to arm us with information so we can decide how much surveillance our pouches need, he then asked us if we had any questions.
Q: In my experience pouch owners are very attuned to changes in pouch function, does this often drive pouch surveillance?
A: Yes – absolutely. Opportunistic surveillance is another option.
Q: How do I know if I am high risk? My colon was removed after long-term ulcerative colitis.
A: After the colon has been removed it is checked for cancerous or pre-cancerous cells and you will have been told if any were present and it will be on record.
Q: Is the advice different if your pouch is for FAP not UC?
A: Yes – if you have had a pouch for FAP you are considered high risk and so need your pouch checked yearly.
I had my pouch in 1999 and it has never worked properly, now I have yearly surveillance it has been put down to Crohns like disease, what can you advise?
Originally being diagnosed with Ulcerative Colitis and then with Crohns in the small bowel is not uncommon, biological treatments for Crohns are one treatment option.
The presentation slides for this session can be found here: Pouch Surveillance
2. The Future of Pouch Surgery
“Never make predictions, especially about the future” – Casey Stengel
Mr Gosling began by talking us through the timeline of important milestones in pouch surgery.
1846 – William T. G. Morton (1819-1868) began doing surgery in the “Ether dome”
Late 19th century – Joseph Lister (1827-1912) began using Aseptic Surgery
1978 – Sir Alan Parks invented the Ileal pouch
1981 – Semm Germany, Laparoscopic (keyhole) surgery is perfected
Mr Gosling explained that keyhole surgery is an improvement on traditional surgery as it involves less trauma and with smaller cuts comes quicker recovery times and fewer/smaller scars. But how can this be improved upon? Robotic surgery.
In Robotic surgery the surgeon sits down so doesn’t get so tired and has 3D vision and depth perception. The surgeon remotely controls the robot using four arms and a camera, the arms have a good range of movement and almost replicate the wrist, they are very dexterous and precise while also eliminating any tremor. Robotic surgery allows surgeons to practice and train on a simulation, surgeons can improve their scores until they are ready to perform actual operations. All data from robotic surgery is captured and assimilated and this can be used to guide operations in the future where an augmented reality is created, and a map can be superimposed on the surgery.
Although robotic surgery has many advantages Mr Gosling explained it also has some disadvantages, the surgeon cannot feel how hard they are pressing as the arms do not provide any feedback, it is cumbersome to set up and expensive . This is difficult to justify as there is no evidence to support any long-term benefits to the patient when using a robot instead of regular surgery, but it has shown to be of most use in pelvic operations in overweight men, as they have a small pelvis.
However, despite the disadvantages Mr Gosling was keen to emphasise how much surgeons like robotic surgery and over the last 10 years the number of operations done robotically in the USA has increased from 130,000 to one million. My Gosling is hopeful that in the future costs will decrease as the robot would allow expert surgeons to perform proctor surgery anywhere in the world by dialling in using the robot.
Another advancement in pouch surgery is the use of Florescence so that for example, the ureter glows in the dark and is not damaged during pouch surgery.
Q: Does robotic surgery take longer?
A: Yes – especially at the start, as did keyhole surgery to start with. In time, as surgeons practice, the time taken comes down.
The presentation slides for this session can be found here: The Future of Pouch Surgery
11:55 – Some Personal Stories Q&A– Mick Goddard, Helen Woodley and Sheena Fisher-Hutchins. Session led by Angie Perrin – Clinical Lead, Innovation, Salts Healthcare
The session took the form of a question-and-answer session, with Angie asking the questions and everyone answering.
Q: Briefly describe the circumstances which led up to your surgery?
Mick – My Ulcerative Colitis grew steadily worse and in 1994 I ended up in hospital for 6 weeks under the care of Dr Jewel.
Helen – I had endometriosis then two babies within two years, then I was very poorly spending a month in hospital, including a week in intensive care, during which time my colon was removed.
Sheena – I had been ill for quite a long time and I was in and out of hospital. Although my UC was only in the end section of my colon it was still awful, so I opted to have pouch surgery.
Q: What is the best thing about having had pouch surgery?
Sheena – Having my life back, I had an ileostomy for 12 months which was okay and then pouch surgery which worked really well!
Helen – Fitting into normal clothes! No leakage, no soreness around the stoma. My stoma nurse bullied me slightly into having pouch surgery and I am so glad she did. Two years after my pouch surgery I unexpectedly became pregnant which did not change my pouch function, I was recommended a caesarian which went to plan. I have also only had one bout of pouchitis in 23 years!
Q Do you have any lifestyle issues?
Mick – I have been abroad many times and flown which has not caused any problems for me, although I don’t drink any more, when I did any amount of drink would get me drunk, but my pouch is fine. When I first had my pouch roast potatoes and chips caused pouchitis. Overall my pouch hasn’t stopped me from doing anything, when I used to work in London, I would commute from 5.20am – 6:30pm and not go to the loo at all. I have a few medical conditions so I take lots of medication, but I don’t take loperamide.
Sheena – I always carry cream, wipes and PooPouri in my bag, and I find stress makes my pouch work more often. Fruit and veg can cause me bloating and wind and I avoid tomatoes completely as they give me problems. I take two loperamide in the morning and two before I go out if I go out the in evening. I used to get a lot of soreness, but Bepanthen nappy cream really helps, even though it makes pants go yellow!
My routine when I go to the loo is: spray first, then go and use toilet paper and finally put on Bepanthen.
Helen – I live half in the UK and half in Portugal, when I had an ileostomy, it inflated on the plane so I would wear an elasticated skirt, but my pouch isn’t affected at all. When going abroad I take my own toilet roll and baby lotion. I often find it is mind over matter, if I have to wait to go I can, I also don’t need to take loperamide. Although I can’t eat pips or seeds, dried fruit or chopped tomatoes I can generally eat anything else with no problems which is fantastic.
Q: Do you ever go to the loo then immediately need to go again?
Sheena – Yes, when I have gone for the first time I stand-up, sit down and rock around to check if I need to go again!
Q: What follow-up have you had after your pouch surgery?
Sheena – I have had one pouchoscopy, I should probably get one soon!
Mick – I am due one next year, I can’t remember when I last had one.
Helen – I had one every two years until 2018, now it has reduced to one every 5 years if there is nothing wrong.
Q: Did you have any problems with your pouch when you first got it?
Mick – Yes, the early years were difficult, and I had lots of frequency, but I learned to live with it and manage my pouch.
Angie explained that the pouch is considered new for up to 5 years, you learn how it functions and your pouch adapts, to your lifestyle. There are many different things to try such as loperamide and liquid loperamide, you can work with nurse specialists and other pouch owners to develop a plan A, plan B, plan C and find out what works best for you.
Following this session everyone that wanted to shared their own personal story with their neighbour.
12:30 – Lunch – Sandwiches, cake and fruit and an opportunity to meet and chat with other pouch owners and their partners
13:10 – The Kangaroo Club Update followed by AGM – Laura Dunn
13:30 -Maintaining Good Pouch Function over Time – Kim Gorrisen: Consultant Emergency Colorectal Surgery, OUH NHS Foundation Trust
Miss Gorrisen started by saying it was an absolute pleasure to meet so many people with pouches, she then went on to explain that she been at OUH for four years and her main interests are emergency surgery and pelvic floor function.
Miss Gorrisen began talking about what normal bowel function is, there is a lot of variation in normal even in people who have not had pouch surgery, with people going from 7 times a day to once every 7 days – as long as you are happy with your function then it can be normal.
Miss Gorrisen then explained what each section of the digestive track does to help us better understand our bodies.
The Large Bowel absorbs about 300-1000ml per day of liquid which solidifies feces, it contains thousands of bacteria which is important for digestion and is used for storage.
The Rectum is also used for storage and tells us when you need to open your bowels.
The Anal Canal differentiates solid, liquid and air to help us control our continence.
Miss Gorrisen talked us through how having a pouch influences our habits.
Not having a colon means less absorption and less storage.
The Anus should not be affected but there could be surgical damage to the nerves and sphincter muscles.
Because the surgery results in less sensory mucosa it can become difficult to differentiate between air, liquids and solids.
Pouch surgery can also come with complications, such as leaks or fistulas.
The common problem (that nobody talks about) is Fecal incontinence (FI) or leakage from the back passage. Miss Gorrisen told us that 10%-15% of all people have problems with continence with 6.5 million people affected in the UK and 100-500 new patients treated in Oxford each year.
Miss Gorrisen took a look at what is ‘normal’ pouch function, comparing 370 patients after 10 years.
Nightly bowel motions are rare in people with a colon, but very common in those without. Having a pouch also changes how long you can wait, most people with pouches can’t hold for longer than 15 minutes. Despite this 94% of the people surveyed were still very happy with their pouch.
Miss Gorrisen went on to look at why the risk of fecal incontinence increases if you are a woman or older when you had your operation.
As we get older our muscle strength deteriorates, this can be worsened by diabetes which damages the nerved of the pelvic floor, the menopause as hormones change, and treatments such as radiotherapy and surgery.
Miss Gorrisen explained that our pelvic floor muscles are so important in preventing incontinence, so we must use them, “if we don’t use it, we lose it”. Miss Gorrisen recommended:
Pilates
Kegles – mainly for women
Pelvitone – but it doesn’t teach you how to use your pelvic floor
Elive – connects to an app on your phone and tells you how hard you are squeezing
Perifit – you use your pelvic floor to play a game
Our diet is very personal and what effect different foods have on you are very personal and can change over time. Artificial sweeteners, such as sorbitol make most people go more. Caffeine, fizzy drinks and alcohol, particularly beer, have all been known to have a negative effect on the pouch. Some fibers are soluble, and some are not and this effect different people in different ways, it is about finding out what works and what doesn’t work for you. Miss Gorrisen reassured us that by trying different things and experimenting with your diet you will not damage the pouch.
Miss Gorrisen started to describe the Gastro-colic reflex. Miss Gorrisen explained that food is in transit in our bodies for 6-8 hours, it is in the stomach for 2-4 hours and the small bowel for 4-6 hours, this slows down when the colon is removed. However, food moving into the small bowel can trigger an urgent need to go 20-30 minutes after eating.
This can be addressed by taking loperamide which comes in different strengths and different forms: syrup, capsules and liquids. The anti-depressant, Amitriptyline, can be taken at a low dose to dampen the reflex of your gut and slow everything down. Metamucil fiber supplements can be taken to bulk up your stool and reduce this reaction.
There are lots of different products about now to address, incontinence including new technologies such as Shreddies incontinence underwear and plugs which Miss Gorrisen recommended for occasions such as running and horse-riding. The Flush app tells you the location of public toilets nearby. Another method Miss Gorrisen told us about was the sacral nerve stimulation which was pioneered in the mid-90s and involved electrical stimulation of nerves that supply the bowel and muscles, under local anesthetic, to reduce fecal incontinence. It is currently in the test phase and has only been tested on two people with pouches, but shows promising technique. Another option is always to have a stoma.
Because pouch liquid is more acidic than for those with a colon this results in sore skin. Other causes of dermatitis are excess moisture from perspiration, urine and faeces, chemical irritation from soaps, mechanical damage from wiping, rubbing and scratching or bacterial or fungal infections. Soaps can be really aggressive so try to avoid them, ensure that when you use wet wipes you only use baby wipes with no alcohol and no perfume. ‘Japanese’ toilets can really help this problem and work really well for people with pouches. Miss Gorrisen told us to ensure we wear breathable underwear to help with skin soreness.
Miss Gorrisen informed us that the number of people suffering from ulcerative colitis has increased but the number of people having a colectomy has gone down – this means we are getting better at medicating UC and the number of people having pouches have gone down. This could be because the stigma of having an ileostomy has reduced due to influencers and changing attitudes.
If you have difficulty emptying your pouch if is worth remembering that your body has been developed to crouch, try to use your muscles in a brace and pump action. Get up and move around then sit back down again. If you continue to struggle one option is using Qufora irrigation which uses a small amount of water to flush out your bowels.
Miss Gorrisen finished by concluding that small changes can make big difference. 10% of all people have incontinence so be brave and talk about it and that you should always dare to ask for help. The following people are a good place to start:
Pouch nurses
Oxford pelvic floor team
GP
Community incontinence services
Gastroenterologist/surgeon
Q: Is it okay to use an anal plug when you have a pouch?
A: Don’t use an anal plug for the first 6 months after surgery. Make sure you put it in yourself, so you can feel it’s working fine and not causing any problems.
The presentation slides for this session can be found here: Kangaroo Pouch Function
14:25 -The Healing Power of Mindfulness – Dr Louise Hankinson: Consultant Clinical Psychologist OUH NHS Foundation Trust, Breathworks accredited teacher
Dr Hankinson started by saying she knew it was hard to open a paper without reading about mindfulness, but how can we practice it? After all it is pretty easy to be mindful when you are sat by a lake, but far less easy in normal day-to-day life.
Dr Hankinson explained that mindfulness can also result in a bad reaction and feel unpleasant if you just sit and think about what is worrying you. She then invited us to try and exercise:
Notice 5 things in/about the room and note them down in your mind
Close your eyes and note down 5 different sounds
Lastly note down 5 areas of touch, 5 points of contact between your body and something else
Open your eyes and come back to the room
Dr Hankinson then asked us what the experience was like? There is no right or wrong answer.
Calming
More aware of myself and how my body feels sitting in the chair
Aware of my breathing
Aware of my individual senses
Dr Hankinson explained that the exercise gave our thinking brains a break as it gave us a small task, and our brains love a task, while focusing on three of our senses.
Dr Hankinson then went on to discuss ‘what is mindfulness?’, giving us two definitions, one from Jon Kabat-Zinn and one from Breathworks.
Mindfulness involves paying attention in a particular way:
on purpose,
in the present moment,
nonjudgmentally.
– JON KABAT-ZINN
The Breathworks definition is:
“By practicing mindfulness, we are bringing our awareness to our experience in the present moment, including sensations, thoughts, and emotions. Through this we can choose to respond, rather than react, to whatever shows up.”
But why is it important? We are very rarely present, often somewhere else (in our minds), therefore we can miss so much of life. In this day and age we are constantly practicing distraction, so therefore we get really good at it, this means we don’t multi-task, we just do everything badly.
Breathworks suggest we focus on the breathing; it is always there so you can always follow it and use it as an anchor.
Dr Hankinson then took us through a second exercise:
Put a hand on your chest and a hand on your belly and breathe
Notice what is happening to you
She asked us who can feel most under their top hand and who can feel most under their bottom hand?
The lungs are triangular, with the diaphragm sitting underneath, as the diaphragm pushes down it pushes on internal organs and pushes out the belly. Dr Hankinson suggested we look up Belly Breathing on the internet as it has been proven to trigger a relax response and calm you.
We then did another exercise:
Put hands on your lap
Breathe
Make a tight fist with one hand, what happens to your breathing?
Release the tension in your hand, what happens to your breathing?
Breathe into your hand (whatever that means to you)
Dr Hankinson explained to us that creating tension in the body impacts your breathing and when you release that tension your breathing lengthens and relaxes. Breath is our signal to the brain that everything is okay and there have been lots of studies that suggest that breathing can:
Reduce stress and anxiety
Increase resilience, creativity and productivity
Improve communication and relationships
Improve decision making
Alleviate pain, psoriasis, depression, IBS, symptom reduction,
Improve sleep
Increased immune function…
When you are diagnosed with an illness you are often living in threat mode. Mindfulness is not:
A quick fix
Making our thoughts go away
Getting rid of stress completely
Zoning out
Fluffy, touchy-feely, nonsense
Tied to any religion
Easy, comfortable
Achieving, or striving
Dr Hankinson told us that sometimes when she drops into what is going on with her mental health it is quite painful, we spend so much of our lives on auto pilot that when we actually feel it can be quite painful.
Dr Frankl said “Between stimulus and response there is a space. In that space is our power to choose our response. In our response lies our growth and our freedom.”
Mindfulness is about creating more of these gaps and making sure our emotional regulation system is working properly.
Very often we go to from the threat system to the drive system and completely miss the soothing system. When the body is in the soothing system the body releases its natural opiates, but how can we access it?
Laughing
Stroking an animal
Intense bonding situations
Mindfulness
Exercise can be drive mode, threat mode or soothing, it depends why you do it. If you do one thing at a time and with full awareness you are being mindful.
Dr Hankinson emphasized the importance of compassion; we often respond kindly to the suffering of others but struggle with offering it to ourselves. How often do we say to ourselves, ‘this is really hard, no wonder you are struggling’? Everything is also a bit easier when you know you are not alone.
Dr Hankinson recommended that we do a 3-minute breathing space exercise to create a full stop or comma in your day.
Sit up straight with your feet flat on the floor
Close your eyes
Turn awareness to yourself and notice, but do not try to change, how you are:
What are your thoughts?
What are your emotions?
Have you got any strong sensations in your body?
Become aware of how you are breathing, in your next in breath and out breath
Notice changes in your body as you breathe and track them
Let go of any judgement you have about what you notice, just be with your breathing
Bring awareness back into your body
Perhaps notice your feet on the floor, contact with the chair
Expand awareness to the sounds in the room
Bring that feeling back into your day
Open your eyes
The presentation slides for this session can be found here: Kangaroo – mindfulness
This session was inspired by the Red Lion Group who recommended Dr Yoram Inspector from St Marks Hospital last year, some of his presentations are available online and are linked to below:
The Relationship between your Gut and your Brain: https://www.youtube.com/watch?v=o6858WJ71KI
The Psyche and the Gut: https://www.youtube.com/watch?v=YF-I2gxqj1s&list=PLe1Qgfe34uSM_9h9lLvKSc1KBgzWV3T0o
15:10 Break-out Sessions – Based on hopes for the day
The breakout sessions were:
Mindfulness with Dr Louise Hankinson
Living with a pouch and specific queries
15:40 Question and Answer Session – Fran Woodhouse, Simon Turley: Senior Specialist Nurses, Colorectal Nursing Team, OUH NHS Foundation Trust and Angie Perrin: Clinical Lead, Innovation, Salts Healthcare
Q: I am diabetic and I have found that some of my tablets do not get absorbed occasionally, this has made me wonder how many medications regularly don’t get absorbed and how can you tell?
A: Hard coated antibiotics are often difficult to absorb. It depends where the pill is absorbed, higher up in the bowel or lower down? Slow-release medication is not good for pouches. Pharmacists often have a good database on what can and cannot be absorbed so it is good to ask them.
Q: Given that people with pouches have difficulties with absorption should we be looking for any vitamin deficiencies?
A: At Oxford we recommend having a yearly blood test, and there are 5 things to look out for in this test:
Full blood count
Urea and electrolytes
Ferritin
B12
Liver function test
16:15 – End
There was plenty of opportunity to meet and chat with (other) pouch owners and their partners during the day.

Fran Woodhouse, Simon Turley: Senior Specialist Nurses, Colorectal Nursing Team, OUH NHS Foundation Trust and Angie Perrin: Clinical Lead, Innovation, Salts Healthcare
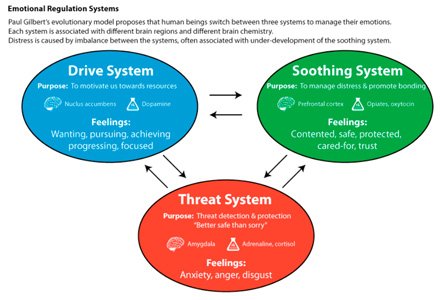
Emotional Regulation System

Dr Louise Hankinson: Consultant Clinical Psychologist OUH NHS Foundation Trust, Breathworks accredited teacher

'Normal' Pouch Function

Kim Gorrisen, Consultant Emergency Colorectal Surgery, OUH NHS Foundation Trust

Lunch and an opportunity to meet and chat with other pouch owners and their partners

Mick Goddard, Helen Woodley and Sheena Fisher-Hutchins.

Mr Jonathan Gosling, Colorectal Registrar, OUH NHS Foundation Trust

Mr Jonathan Gosling, Colorectal Registrar, OUH NHS Foundation Trust
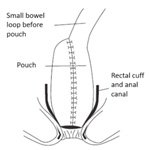
J Pouch

Hopes for the Day

Correct Position for Opening your Bowels
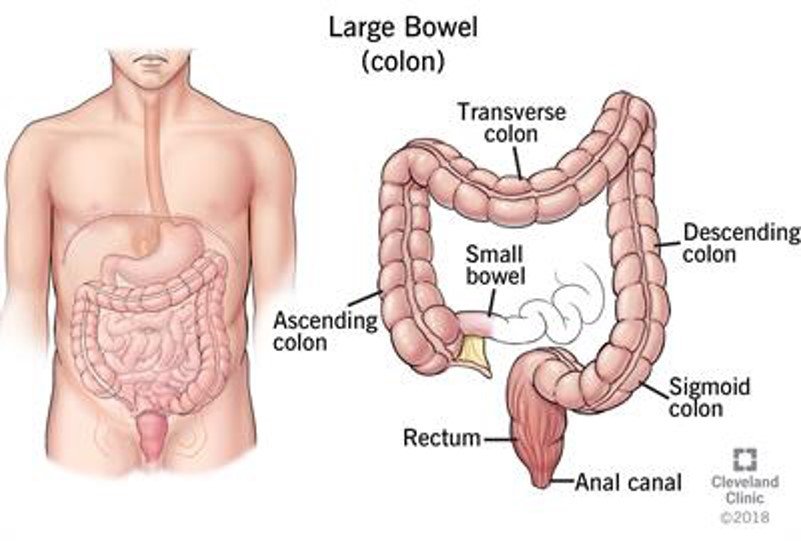
Large Bowel
